Blog

Anxiety is a deeply complex emotional experience that affects not only those who suffer from it directly but also the people who care about them. When someone you love is struggling with anxiety, your instinct is likely to help—to comfort, to fix, to protect. However, despite your best intentions, your support can unintentionally become a barrier to healing if it reinforces the very behaviors that maintain their anxiety. Learning how to support a loved one effectively without enabling unhealthy habits is a delicate balance, but it’s one worth mastering.
Understanding Anxiety at Its Core
Anxiety is more than feeling “worried.” It’s a multi-dimensional condition that encompasses emotional, cognitive, and physiological components. It can be generalized or specific to certain triggers, such as social interactions, health concerns, or traumatic memories.
- Common symptoms of anxiety include:
- Racing thoughts or constant worry
- Physical tension, chest tightness, and restlessness
- Avoidance of certain places, people, or responsibilities
- Reassurance-seeking or compulsive behaviors
- Emotional outbursts or withdrawal
These symptoms are not a result of weakness or attention-seeking. They are manifestations of an overactive threat detection system in the brain—one that sometimes misfires, perceiving danger where none exists.
The Anxiety-Avoidance Cycle
A key driver of persistent anxiety is the cycle of avoidance. A person feels anxious about a particular situation (say, attending a social event), so they avoid it. This avoidance reduces their immediate distress, which positively reinforces the behavior. In essence, the brain learns: “Avoiding this makes me feel better; therefore, I should keep avoiding it.”
When loved ones intervene to help someone avoid anxiety triggers—by making excuses for them, taking over responsibilities, or providing constant reassurance—they become a part of this reinforcement loop. While it may feel like kindness in the moment, it inadvertently teaches the anxious person that their fears are valid and unmanageable.
Common Unhealthy Coping Mechanisms in Anxiety
To truly support someone, we must recognize which coping behaviors, although soothing in the short term, are ultimately unhelpful. These include:
- Chronic avoidance: Refusing to engage in work, school, or social functions
- Excessive dependence: Relying on others for every decision or action
- Compulsive behaviors: Checking, seeking reassurance, or repeating rituals
- Substance use: Using alcohol or drugs to manage stress or panic
- Therapy resistance: Refusing professional help out of fear of discomfort
These behaviors are understandable but unsustainable. If we want to help our loved ones truly heal, we must gently challenge these patterns—not accommodate them.
What Supportive (Yet Boundaried) Help Looks Like
The key to supporting someone with anxiety lies in validation, encouragement, and boundaries. Below are actionable strategies to practice compassionate, non-enabling support:
1. Validate Feelings Without Confirming Fears
Saying things like “I can see this is hard for you” or “It makes sense that you’re feeling anxious right now” validates the person’s emotional state. Avoid phrases that confirm distorted beliefs, such as “You’re right, that situation is dangerous.” Your role is to be empathetic but not reinforce anxiety-driven interpretations.
2. Encourage Gradual Exposure
Exposure therapy is one of the most effective treatments for anxiety. Support your loved one by encouraging small, manageable steps toward feared situations rather than allowing them to avoid those experiences entirely. You might say: “Let’s try going together for just 10 minutes—you can leave if it feels overwhelming.”
3. Encourage Gradual Exposure
Gradual exposure to feared situations is a central strategy in many therapies for anxiety. You can encourage them to face small challenges, accompany them if necessary, but resist the urge to avoid them.
4. Promote Seeking Professional Help
Anxiety may require therapeutic intervention, and your role as a supporter can be to encourage and normalize seeking help. You can offer to help them find a therapist, accompany them to the first session, or simply ask how the process is going.
5. Take Care of Yourself
Caring for someone with anxiety can be emotionally draining. Establish self-care times, seek support from others, and, if necessary, consider seeking therapy yourself to manage the emotional burden.
Specific Strategies for Common Situations
When They Call You Repeatedly Seeking Reassurance
This habit can become addictive for someone with anxiety, because each time they are reassured, the relief reinforces the behavior of asking.
What to do: Set specific times to talk or a limited number of messages per day. Encourage the person to practice breathing techniques or write their thoughts in a journal before calling you.
When they want you to cancel events for them
What to do: Encourage them to face the event. You can offer to accompany them, but don't assume the role of manager. For example, say, "I'm sure you can do this. If you decide to go, I fully support you."
When they avoid all social contact
What to do: Invite them to participate in small, non-threatening plans. Avoid insisting if the answer is no, but keep the invitation open and acknowledge their achievements when they are encouraged.
What not to do
- Don't trivialize their experience: Phrases like "it's just anxiety" or "we all go through it" minimize real suffering.
- Don't become their therapist: Listening and supporting doesn't replace professional work. Don't make decisions for them.
- Don't lose your identity in the relationship: Avoid completely changing your life or sacrificing your emotional well-being in the name of support.
The Importance of Long-Term Change
Supporting someone with anxiety isn't a matter of days or weeks. It's a process that requires patience, consistency, and a great deal of compassion. Your role isn't to cure the person, but to help them discover that they can trust themselves, even in the midst of discomfort.
Every time you choose not to reinforce a bad habit, you are contributing to the development of internal coping tools. At first, the person may be upset, feel misunderstood, or rejected. But over time, they will understand that true help lies not in avoiding discomfort, but in learning to confront it.
Final Reflection
Loving someone with anxiety is an act of dedication and resilience. It requires balance: being present without overprotecting, supporting without replacing, validating without perpetuating fear. It is difficult, but deeply transformative.
If you are in this process, also recognize your own achievements. Your role is crucial in that person's journey to healing. And remember: the goal isn't to eliminate anxiety, but to teach it can be managed with courage, love, and autonomy.
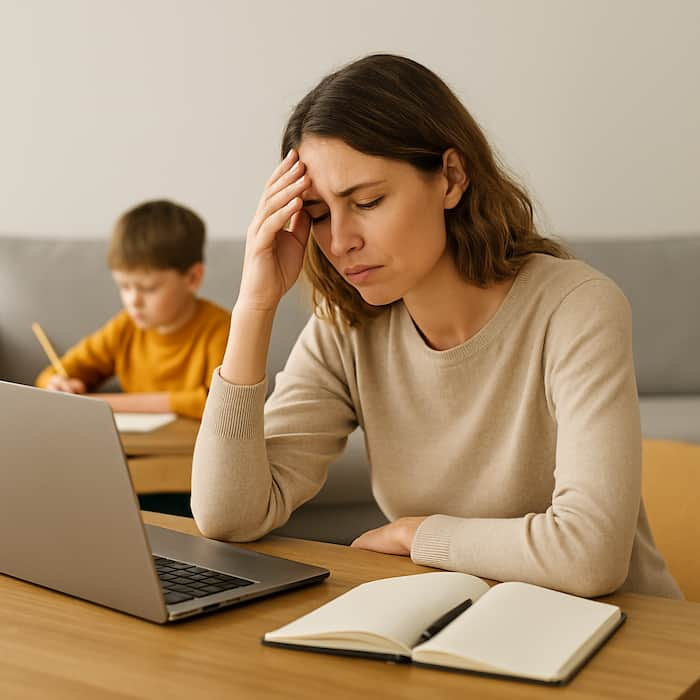
Parental guilt is a deeply rooted emotion that affects millions of parents around the world. It often arises when we try to balance our professional responsibilities with the desire to be present, loving, and attentive parents. This sense of guilt can manifest in thoughts like: "I don't spend enough time with my children," "I'm failing as a parent because I work too much," or "I'm sacrificing my family for my career." While these concerns are valid and reflect genuine love for your children, they can also become an emotionally draining burden that impacts your personal well-being and the quality of your family life.
Fortunately, therapy offers a safe and effective space to explore, understand, and overcome this guilt. In this blog, as a psychologist specializing in various forms of therapy, we’ll explore how parental guilt manifests, its emotional roots, and how therapeutic techniques can help you build a more balanced, compassionate life centered on what truly matters.
Understanding Parental Guilt: Where Does It Come From?
Parental guilt doesn’t appear out of nowhere. It generally stems from a mix of social, cultural, personal, and emotional factors. The most common include:
- Idealized societal expectations: The media, social networks, and popular culture often project images of “perfect parents” who are always available, cook every meal, attend every school event, and maintain a spotless home. Comparing yourself to these unrealistic standards can lead to chronic guilt.
- Internalized critical beliefs: Many parents hold onto internal scripts such as “my kids should always come first,” “I’m selfish if I think of myself,” or “I must sacrifice everything for my family.” Though born from love, these beliefs can become unattainable and self-punishing demands.
- Unresolved childhood experiences: If you grew up with absent, neglectful, or hypercritical parents, you might have promised yourself to be the opposite. This can push you to overextend yourself and feel guilty whenever you fall short of your ideal version of parenting.
Signs Parental Guilt Is Affecting Your Well-being
Feeling occasional regret is normal. But when guilt becomes a predominant emotion, it can lead to negative outcomes such as:
- Constant anxiety about the time spent (or not spent) with your kids.
- A pervasive sense of not doing enough, even when giving your best.
- Difficulty enjoying free time or disconnecting from work.
- Irritability or unexplained sadness.
- Overcompensating behaviors like excessive gift-giving or leniency to make up for perceived absence.
How Therapy Helps You Overcome Guilt
1. Acknowledging and validating your emotions
Therapy begins by validating your experience. It’s entirely normal to want to be more present and to care deeply about your children’s well-being. In a therapeutic space, you can express these emotions without judgment. You’ll learn that feeling guilty doesn’t necessarily mean you’re doing something wrong—it simply means you care deeply.
2. Reframing irrational beliefs
Using approaches like Cognitive Behavioral Therapy (CBT), your therapist helps you identify automatic thoughts like “If I’m not home all day, I’m a bad parent.” These thoughts are challenged with real evidence: Are your children cared for? Do you connect emotionally when you’re present? Are you modeling the value of hard work?
Reframing can relieve guilt and promote a healthier mindset: “I don’t need to be perfect, just meaningfully present.”
3. Strengthening parental self-esteem
Many parents judge themselves harshly but rarely acknowledge what they do well. Therapy actively helps you identify your strengths as a caregiver. You’ll learn to speak to yourself with compassion—the same way you’d speak to a friend.
4. Establishing priorities and healthy boundaries
A key part of therapy involves clarifying your values and aligning your decisions with them. If you value family, how can you structure your time to be emotionally available without abandoning your professional goals?
This includes learning to say “no” when necessary—both at work and in your personal life—and setting up routines that honor both your needs and your children’s.
5. Developing emotional regulation techniques
Guilt often comes bundled with stress, anxiety, and fatigue. Techniques such as mindfulness, breathing exercises, journaling, and gratitude practice can help you manage overwhelming emotions and stay grounded.
Everyday Practices to Reduce Parental Guilt
In addition to therapy, there are simple habits you can incorporate into your daily life to foster emotional balance:
- Focus on quality over quantity: Spending the entire day with your children while being distracted doesn’t foster connection. It’s more valuable to share 30 minutes of genuine play, reading, or conversation than to be together all day without real engagement.
- Use realistic self-assessment: Ask yourself each night: Did I do something today that contributed positively to my family? Acknowledge even the small actions—making breakfast, giving a hug, or listening attentively.
- Replace guilt with gratitude: Instead of thinking “I wasn’t with them this afternoon,” try reframing: “I dedicated time to work so I can provide for them, and tomorrow I’ll have a special moment together.”
- Model self-care: Showing your kids that you need rest, exercise, or time for hobbies teaches them that self-care is part of healthy family life.
- Lean on your support network: Talk to other parents and share your feelings. You’re not alone. Community can help you realize your struggles are shared and there are healthier ways to cope.
The Role of Self-Compassion in Parenting
Self-compassion is a powerful tool widely used in therapy, especially in Compassion-Focused Therapy. This practice invites you to treat yourself kindly—especially when things go wrong or you face hard days. Instead of beating yourself up for not being a “perfect parent,” try saying: “I’m doing the best I can with what I have, and that’s enough.”
This attitude not only benefits your mental health—it also has a positive effect on your children. A parent who treats themselves with respect and care is better able to raise emotionally resilient children.
Is Perfect Balance Even Possible?
The honest answer is no. Work-life balance is dynamic, not static. Some weeks your job will demand more, and other weeks you’ll prioritize home life. What matters is the consistent intention to nurture your relationships and your well-being without sacrificing one for the other.
Remembering this can help you let go of the idea that you need to be “everything for everyone, all the time.” Instead, embrace the possibility of being enough, being flexible, and being human.
Conclusion
Overcoming parental guilt doesn’t mean ignoring your responsibilities or caring less—it means learning to manage them from a place of love rather than pressure. Therapy is a powerful tool to help you understand yourself better, let go of limiting beliefs, and build a life where your family and career coexist with greater harmony.
If you recognize yourself in many of the emotions described here, remember that you are not alone. Asking for help is not a sign of weakness—it’s a sign of emotional strength and commitment to your well-being and that of your children.
Would you like personalized guidance to work through parental guilt and build a healthier routine? Reach out to us here. We’re here to support you every step of the way.

Depression is one of the most common and complex psychological conditions affecting millions of people worldwide. It’s often marked by persistent feelings of sadness, loss of interest in everyday activities, extreme fatigue, and difficulty concentrating or making decisions. Yet, one of the most puzzling and frustrating aspects—for both those suffering and their loved ones—is the refusal or resistance to accept help. Why would someone in pain reject support that could ease their suffering? This seemingly contradictory behavior is rooted deeply in human psychology and the very mechanisms of depression itself.
1. Harsh Self-Criticism as an Internal Obstacle
One of the defining features of depression is an extremely harsh and judgmental inner voice. Depressed individuals often see themselves as burdens, as people undeserving of attention or support. This isn’t an exaggerated belief but a very real part of how depression alters one’s self-perception.
Thoughts such as “I don’t want to bother anyone” or “They have their own problems” are common. This internal narrative can become so overpowering that it suppresses any instinct to seek support. Accepting help may feel like admitting weakness, or worse, like manipulating others for attention.
2. Lack of Energy and Motivation
Another major barrier is the emotional and physical exhaustion that comes with depression. Simple tasks—like getting out of bed, showering, or preparing a meal—can feel insurmountable. Now imagine how overwhelming it can be to reach out to a friend, schedule a therapy appointment, or even respond to a text message offering help.
Accepting help often involves making decisions, explaining one’s needs, or engaging with others—activities that demand energy many people with depression simply don’t have. It’s not about not wanting to get better; it’s about being emotionally and physically paralyzed.
3. Shame and Stigma
Despite growing awareness, depression still carries a heavy stigma. For many, admitting they need help is equivalent to acknowledging that they are broken or incapable of managing their own lives. This perception fuels feelings of shame and guilt.
Our culture’s emphasis on “being strong” or “pushing through it” reinforces the belief that seeking help is a weakness. For men, this is often intensified by traditional norms around masculinity, which equate emotional expression with fragility. The result is a hesitancy to open up or accept assistance for fear of being judged or misunderstood.
4. Fear of Vulnerability
Accepting help requires vulnerability. It means allowing others to see your emotional wounds. For many people, this exposure is terrifying. Vulnerability demands trust, and trust—in oneself, in others, in the future—is often in short supply when someone is depressed.
There’s also the fear of being misunderstood. Depression is profoundly personal and often difficult to articulate. People may have past experiences of opening up only to be dismissed or minimized, leading to a protective silence: “No one will understand anyway.”
5. Cognitive Distortions: When Help Feels Like a Threat
From a cognitive-behavioral perspective, depression is associated with distorted thinking—ways of interpreting reality that are biased or irrational. These distortions can lead someone to interpret even well-intentioned gestures of help as veiled criticism or confirmation of failure.
For example, if a friend offers to accompany someone to therapy, it might be perceived as: “They think I’m crazy,” or “They don’t trust me to do it on my own.” These thoughts, while distorted, feel absolutely real to the person experiencing them and reinforce the instinct to withdraw.
6. Fear of Hope
Paradoxically, another reason someone might resist help is the fear of hope itself. When someone has been depressed for a long time, the pain can become familiar, even comfortable. Imagining that life could improve requires opening up to hope—and with hope comes the risk of disappointment.
Accepting help means entertaining the idea that things might change. But for someone who has faced repeated failures or false starts, the fear of yet another letdown can be too much to bear. It’s a painful form of self-protection: “If I expect nothing, I won’t be hurt again.”
What Can Therapy Do?
Understanding these barriers is essential for addressing them effectively in therapy. A therapist’s role is not simply to provide solutions, but to create a space where the person feels safe, seen, and validated. Key therapeutic strategies include:
1. Validate Without Pushing
Therapists should demonstrate sincere understanding without pressuring the individual to change. Phrases like “It’s okay to take your time” or “I’m here when you’re ready” offer emotional safety without demands.
2. Cultivate Self-Compassion
Using techniques from Compassion-Focused Therapy (CFT), therapists help clients develop a kinder internal voice that sees accepting help as a strength rather than a flaw.
3. Challenge Cognitive Distortions
Cognitive restructuring techniques help clients explore and question irrational thoughts: “Am I really a burden?”, “What proof do I have that no one wants to help me?”
4. Set Small, Achievable Goals
Instead of big changes, therapy can focus on small victories: responding to a message, making a phone call, attending one therapy session. The aim is to build trust in the healing process, one step at a time.
5. Strengthen Support Networks
Therapists can help individuals identify people in their lives who can offer safe, nonjudgmental support. Rebuilding bridges to the outside world is a slow but vital process.
What Can Loved Ones Do?
Family members and friends play a crucial role—but must act with sensitivity. Some helpful actions include:
- Avoid Judgment: Dismissive phrases like “just cheer up” or “others have it worse” are harmful. Instead, validate the person’s experience and offer genuine presence.
- Be Present, Not Pushy: Simply being available—without trying to fix or analyze—can make a big difference.
- Respect Their Pace: Everyone has their own timeline for accepting help. Forcing the issue can backfire.
- Learn About Depression: Understanding the condition helps friends and family respond with more empathy and effectiveness.
Conclusion
Accepting help during depression isn’t a simple decision—it’s a deeply emotional and psychological process. It involves breaking through layers of shame, fear, distorted thinking, and exhaustion. Effective therapy respects these barriers and works gently to dismantle them with compassion and patience.
If you or someone you know is struggling with depression, remember: you are not alone. There are people, tools, and paths that can help. Healing begins not with pressure, but with trust. With the right support and understanding, even the most fortified emotional walls can start to come down.

Childhood is a crucial stage in the formation of our identity, our emotions, and, especially, how we relate to others. The experiences we live during our early years have a profound impact on how we connect in adulthood: in friendships, work relationships, and especially in romantic partnerships. From the perspective of clinical psychology and various therapeutic approaches, extensive research has explored how attachment, emotional security, trauma, and family dynamics shape long-lasting emotional patterns.
This article aims to analyze how early-life experiences can influence the way we emotionally connect in adulthood and how therapy can help us recognize and transform these patterns when they become dysfunctional.
1. Attachment Theory: The Foundation of Bonding
One of the most influential models in understanding human relationships is attachment theory, developed by John Bowlby and Mary Ainsworth. This theory posits that the quality of the bond a child forms with their primary caregivers influences their ability to trust, feel secure, and establish stable relationships in the future.
Attachment styles are mainly classified as:
- Secure attachment: The child feels loved, protected, and cared for. As an adult, they tend to have stable relationships, trust others, and handle autonomy well.
- Anxious attachment: The child experiences inconsistent attention. In adulthood, this may manifest as emotional dependency, a constant need for approval, and fear of abandonment.
- Avoidant attachment: The child learns that expressing emotions is not safe. As an adult, they tend to avoid intimacy and suppress emotions.
- Disorganized attachment: Arises in contexts of trauma or abuse. In adulthood, it may manifest as chaotic relationships, emotional confusion, and difficulty setting boundaries.
Recognizing our attachment style can be a powerful therapeutic tool to understand our reactions in relationships and begin developing healthier bonds.
2. The Role of Family Modeling
During childhood, parental figures act as behavioral models. Through observation, children learn how to handle conflicts, express emotions, and show love or disapproval. If we grew up in a home filled with respect, communication, and affection, we are likely to carry those values into our adult relationships. But if the environment was marked by yelling, indifference, or violence, we may internalize those behaviors as "normal" ways of relating.
For example:
- A child who constantly witnesses aggressive arguments between parents might normalize conflict as an inevitable part of any relationship.
- A girl who grows up with emotionally unavailable parents may develop the belief that her emotional needs are unimportant.
These internalized patterns act as invisible scripts we unconsciously reproduce, even if we rationally want something different.
3. Emotional Wounds from Childhood
Emotional wounds suffered during childhood—such as rejection, abandonment, humiliation, betrayal, or injustice—leave marks that affect our self-esteem, our sense of worth, and our ability to trust. These wounds often manifest in adult relationships through:
- Intense jealousy
- Fear of commitment
- Need for control
- Emotional avoidance
- Difficulty expressing affection or needs
The good news is that, while these wounds may be deep, they do not have to define us forever. With proper therapeutic support, it is possible to heal, reinterpret, and choose healthier ways to connect.
4. Defense Mechanisms and Repetition of Patterns
Many adults repeat relational patterns without realizing it. A person who experienced emotional neglect may feel attracted to cold or distant partners, perpetuating the same kind of pain. This phenomenon, known as repetition compulsion, is common among those who have not processed childhood trauma.
Additionally, we develop defense mechanisms to avoid pain, such as sarcasm, hyper-independence, or submission. While these may protect us in the short term, in the long run, they can sabotage our most meaningful relationships.
Therapy offers a safe space to identify these mechanisms and transform them into tools for emotional growth.
5. Self-Esteem and Sense of Personal Worth
The messages we receive during childhood about our worth—whether we are enough, whether we deserve love, whether our emotions are valid—have a direct impact on adult self-esteem. A person with damaged self-esteem may settle for toxic relationships, feel unworthy of something better, or fear being alone if they set boundaries.
In contrast, those who grew up in environments that validated their identity and emotions tend to form more equitable and healthy relationships.
Rebuilding self-esteem in therapy involves challenging limiting beliefs, constructing a more compassionate internal dialogue, and learning to set boundaries without guilt.
6. Childhood Trauma and Adult Relationships
Childhood trauma—whether physical, emotional, sexual abuse or neglect—can deeply alter emotional development. People who have experienced trauma may exhibit:
- Hypervigilance in relationships
- Difficulty trusting
- Symptoms of anxiety or dissociation
- Attraction to abusive dynamics
Approaches such as EMDR therapy, somatic therapy, or cognitive-behavioral therapy have shown that trauma can be processed and its effects reduced. It’s not about "forgetting" the past, but integrating it from a place of greater awareness and emotional strength.
7. The Role of Therapy in Healing Bonds
Therapy not only allows us to talk about the past but also understand how that past lives in our present. Through a secure therapeutic bond, it is possible to:
- Explore early experiences with compassion
- Identify and question dysfunctional relationship patterns
- Learn new ways to bond
- Heal persistent emotional wounds
- Strengthen self-esteem and emotional intelligence
Additionally, couples therapy can be a powerful tool to work together on difficulties that arise in the relationship due to unresolved childhood histories.
8. Transforming Emotional Legacy
Healing does not mean having had a different childhood, but rather building a more conscious and free adulthood. When we do the necessary emotional work, we can break generational cycles of pain and build healthier bonds, both with our partner and our own children.
Many adults discover in therapy that they can learn to care for, love, and protect themselves in ways they never experienced in childhood. That process, although challenging, is profoundly liberating.
Final Thoughts
Childhood experiences lay the foundation for our adult relationships, but they do not have to dictate our emotional destiny. Through self-awareness, introspection, and therapeutic support, it is possible to break destructive patterns, heal emotional wounds, and build healthier, more respectful, and loving relationships.
Accepting our story is the first step. Transforming it is the great act of self-love.
If you’re ready to begin your own healing process, schedule a session with one of our specialists by visiting our services page.

In everyday life, many people struggle with a constant need for external reassurance: seeking validation from others, needing absolute certainty before making decisions, craving approval to feel worthy, or trying to control every possible outcome. While this habit can feel comforting in the short term, it becomes an obstacle in the long run-limiting emotional freedom, personal growth, and autonomy. At its core, this need often stems from deep-seated insecurities, fear of failure, early experiences of rejection or trauma, and a fragile self-concept.
The good news is that this pattern can be broken. Through therapy, self-awareness, and the cultivation of self-confidence, it’s possible to shift from external dependence to internal security. This article explores how reassurance-seeking shows up in our lives, why it's hard to break, and how therapy can help foster a more empowering sense of self-trust.
Comments Made




Leave your comment